







Sciatica is a common yet debilitating condition that causes pain, tingling, or numbness radiating along the sciatic nerve.
For residents of Dubai, finding effective, long-term relief can be challenging, especially with treatment options often focusing on symptom management rather than the underlying causes.
As a McGill Method Certified Personal Trainer, I provide a science-based, non-invasive approach to sciatica treatment.
With evidence-based techniques developed by Dr. Stuart McGill, one of the world’s leading experts on low back pathologies, I help my clients alleviate pain, restore function, and build resilience against future flare-ups.
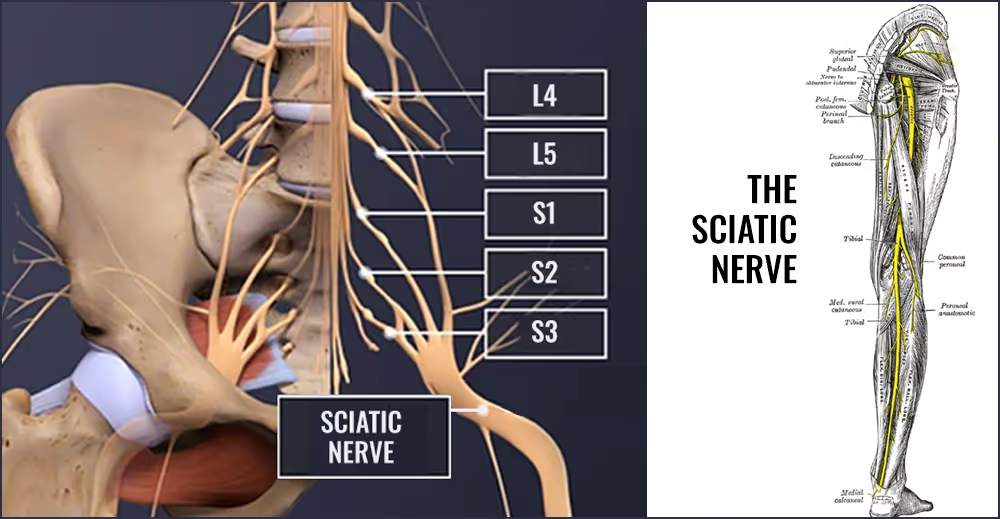
Understanding why sciatica occurs is key to treating it effectively. The majority of cases are linked to herniated discs at the L4-L5 and L5-S1 levels of the lumbar spine. These are among the more mobile spinal joints and they're also subjected to greater load due to their position at the base of the spine.
Forward bending, twisting, and improper lifting techniques place disproportionate stress on these discs making them more vulnerable to herniation.
When a disc herniates, its inner, gel-like nucleus can press against nearby nerve roots, such as the L4, L5, or S1 nerve roots, which are major contributors to the sciatic nerve. This compression or irritation can cause shooting pains down the back and side of the leg, sometimes reaching the foot or toes.
Disc herniation explained by Dr. Stuart McGill
Unlike many approaches that focus only on alleviating symptoms, the goal of the McGill Method is to identify your individual pain triggers, eliminate them from your daily routine, then build an injury-resistant back. It involves the following:
1. A Comprehensive Assessment
After taking a detailed personal history I take you through specific pain-provocation tests to pinpoint the exact causes of your sciatica. This allows us to identify the movements, postures, and loads that aggravate your pain and those that alleviate it.
2. The Elimination of Pain Triggers
Once we know what’s causing your sciatica, the first step is to remove your individual pain triggers from your daily life. I teach you personalised 'spine hygiene' which may involve adjusting how you sit, stand, lift, perform your daily activities and even sleep. This reduces stress on your damaged disc(s) which is essential to allow healing.
3. Building a Resilient Spine
Through precise exercises, we focus on rebuilding spinal stability, first via muscular endurance, then strength. Mobility of adjacent joints such as the hips may also need to be addressed in order to reduce stress on your spine. Your personalised exercise program is designed specifically for the level you're at now, and is progressed at regular intervals.
4. Progressive Rehabilitation
As your pain subsides, we gradually reintroduce more challenging movements to prepare your body for daily activities, sports, or work demands—whatever your goals may be.
Dubai offers numerous therapists and fitness professionals, but what sets me apart is my specialization in the McGill Method (I'm currently the only McGill Method certified practitioner based in Dubai). My unique expertise enables me to:
1. Empower you with knowledge about your condition and teach you how to manage it effectively.
2. Tailor a movement and exercise program specifically adapted to you as an individual.
3. Focus on long-term solutions instead of temporary pain relief.
Moreover, as a personal trainer based in Dubai, I understand the challenges of living in a fast-paced city where long hours, sedentary work, or intensive physical activities can exacerbate sciatica.
I’ll help you to adopt the movement and lifestyle habits that are required for a successful recovery.
 BOOK YOUR CONSULTATION
BOOK YOUR CONSULTATION'I had been suffering from a sciatica for the past two years and despite seeing osteopaths and trying all sorts of pain killers and exercises, I never managed to get rid of it permanently. I got used to living with it, never feeling comfortable, waking up at night etc.
It had become so normal that I hadn’t even mentioned it during my intial consultation with Andy. However, during our first session he immediately noticed something was up. When he realised I had a chronic sciatica he changed my program to focus on that specific problem.
I still thank him every time we meet because not only did my sciatica disappear, but two years down the track, it has NEVER come back - even during pregnancy and after having a baby! So I would more than wholeheartedly recommend Andy for any health and fitness goal you are wanting to achieve.'
—Vanessa Campbell
'For several months , I suffered from back and leg pain that made it impossible to sit or lie down without constantly changing positions. Skeptical at first, I decided to try the unique approach my PT Andy suggested: targeted postural exercises and continuous reminders about maintaining proper movement hygiene.
Through patient and detailed sessions, Andy taught me how to move correctly, avoid harmful movements for my back, and incorporate these new habits into my daily life. His dedication and attention to detail were crucial for my improvement. In just a few weeks my back pain completely vanished. Now, I can sit and lie down without any discomfort.
Andy's expertise and professionalism are unparalleled.I highly recommend Andy’s approach to anyone suffering from similar issues: focusing on posture and movement can work wonders.
Thank you from the bottom of my heart for freeing me up from pain!'
—Angela Grilenzoni
If you’re searching for sciatica treatment in Dubai, you don't need to settle for temporary fixes. I can help you regain control of your life with a proven, research-backed approach that treats the root cause of your pain.
Book a free consultation with me today to find out more.
'I cannot recommend Andy highly enough! Despite being only 24, I suffered from poor posture throughout my adolescence and young adulthood. This, combined with hours spent working on a computer and incorrect form in the gym, led to a severe herniated disc injury. I felt utterly hopeless about being able to sit and work, let alone return to resistance training.
After consulting a doctor, undergoing X-rays, MRIs, and attending several costly physical therapy sessions that provided no significant relief, I decided to turn to Andy, the Back Coach.
Andy's expertise in the human body, along with his extensive knowledge and tailored approach, proved invaluable in helping me make a full recovery. He not only guided me back to my normal life but also helped me safely resume my resistance training routine.
Andy's unwavering support throughout my journey has been truly priceless. If you're struggling with back pain, don't hesitate to reach out to Andy - he genuinely is a miracle worker! Since my recovery, I have confidently referred many friends dealing with debilitating back pain to Andy.'
—Bilel Rais
'I have had a variety of back issues for most of my adult life. I am 57 and have always exercised regularly, but I was at the point where I was taking pain medication daily and regular physiotherapy wasn’t helping to relieve the pain. I was doing an exercise program designed for people with back pain, but I was starting to feel that perhaps it was working against me and I went looking online for a personal trainer who really understood back issues.
In the initial 3-hour session, Andy was meticulous about understanding my history and what kinds of movements both caused and relieved the pain. No other health care provider has taken this kind of time and attention.
The training sessions Andy has put together have been enjoyable, just challenging enough, and with enough variety that they aren’t boring. The app works very well, and Andy has been very responsive to any questions or issues. When something isn’t working for me, he makes suggestions until we find something that helps.
I live in a rural, isolated area so being able to access a personal trainer online is necessary. I wasn’t sure how effective this was going to be, but Andy has unique skills that have made it work very well. It feels very much like we are working together in the same room.Highly recommended!'
—Anne Bennett
'Andy has worked a literal miracle on my back. Before I had almost constant pain and now I have hardly any. His practical approach to strengthening, stretching and movement comes from a place of experience and solid knowledge. My general strength and fitness has also improved so that I can run pain free again. I couldn't recommend him highly enough!'
—Sarah Morter-Laing
'I injured my back 6 years ago and, since then, I've been dealing with chronic pain. My case has become complex and hard to deal with and working with Andy has brought me back confidence and hope in the near future. He has the skills I need the most: PATIENCE, UNDERSTANDING AND DEDICATION (at least in my case, chronic pain goes beyond physical pain, incurring in psychological insecurity and these skills are key), he is KNOWLEDGEABLE and knows how to identify the little imperceptible things that other practitioners don't, and GIVES ME THE EXERCISES that I need for my recovery, not only to improve my back health but my body's physical condition in general. Thank you very much ANDY.'
—Rámon Sánchez Quintanar Ramos
'Andy was absolutely excellent. I've had back issues for years, and I've never been better than after the regiment he arranged.
Not only did Andy point me to what I should be doing, he helped me get rid of some of the exercises I thought were helping that were actually keeping my back injured.
Cannot recommend him enough, super professional, accommodating and personal approach!'
—Eugen Alpeza
'After months with pain in the lower back and trying massages, stretching and abdominal exercises, yoga, physiotherapy which worsened the symptoms, I decided to look for a solution that tackled exactly my problem and found Andy.
After a video call to check expectations and modalities we started with a thorough 3 hrs analysis. I was surprised with which detail this is possible via Zoom and yes, Andy has an experienced eye in observing which type of movements are causing pain and how to modify them.
After that, I received a written summary of the analysis and daily exercises. The program was updated every couple of weeks after checking in trying more and other types of exercises. I still receive my daily workout.
The pain improved quickly with the few adjustments in my daily behavior and the exercises, and after a couple of weeks I was pain free almost always.
Thank you so much Andy for your patience and dedication.
The money here is well spent - for the sake of a pain free life.'
—Jannett Hucke
'I have being struggling with my lower back (L4-L5) since almost three years, I had surgery and stopped feeling the pain through my leg but nothing seemed to really work to stop feeling pain in my back.
I decided to contact Andy for help and I think that was the best idea. I have being doing his back program for almost four moths, and having online sessions every two weeks with him.
I am happy to say that now I have days that I really don't notice my back and I started to do more of the ordinary things that I stopped doing because of my back.
He is an extraordinary professional, always kind and willing to help. If he managed to help me this much in these few months I can't wait to see whats next in the months to come.
Thank you, Andy 🙂'
—Mayte Medina
'I call Andy a miracle worker. Without even being in the same room or running any tests, he was able to diagnose the chronic lower back pain I’d been suffering from for four years.
I had tried every conventional method to relieve my pain—medication, physiotherapy, chiropractic care, acupuncture, deep tissue massages, yoga—you name it. Nothing worked.
As it turned out, I had undiagnosed herniated discs. Remarkably, just by stopping the stretches I’d been doing for years, I experienced immediate relief.
Andy’s thorough approach and easy-to-follow program have made a huge difference in my life. I now feel empowered, in control of my pain, and hopeful about my future. Moreover, I understand my condition and trigger points better, so I am able to work around it.
Although there’s still a long road ahead, I finally see a silver lining. I fully recommend working with Coach Andy and following his program.'
—Najma Khan
'I contacted Andy for the Low Back Pain Rehab Program in January 2024. Two years before, I had injured my back (herniated disc), which led to chronic back pain. Besides the obvious discomfort, I was also fearful of resuming training and potentially reinjuring my back. I came across Dr. Stuart McGill's book, "Back Mechanic," which provided great insights on back pain in general as well as practical advice so as to avoid common mistakes that can aggravate back pain and prevent recovery.
Yet, I felt the need for personalized coaching to ensure I was following the right approach. This prompted me to contact Andy, a McGill Method Certified Practitioner. I began the at-home program, which included daily training, some face-to-face sessions, and online follow-ups. Andy was always attentive to my well-being, listening and ensuring the training progressed according to my capabilities and specific back condition.
Having recently completed the program, I have been free of back pain ever since, and I couldn’t be happier. I've also noticed increased resistance and core muscle strength. Now, I feel prepared to take my training further, so I will continue with a personalized program 💪Thank you Andy!'
—Mara Carloni
'After more than a year of having a back injury that prevented me from doing the sports I wanted and after consulting several specialists, I discovered Stuart McGill and his method for rehabilitating people with back pain. I found Andy on the list of certified practitioners on McGill's website and got in touch with him.
After a very complete assessment and sound advice, I began a rehabilitation program with him. I quickly became able to do movements again that I hadn't been able to do previously and my pain gradually faded until it disappeared completely. This was despite me having had some extremely painful episodes! I admit that I'd been beginning to lose hope about whether I would ever find a solution.
For those who are familiar with fitness training: I went from writhing in pain while sneezing to being able to swing a 32 kg kettlebell without pain! I built up to this in a progressive, safe and effective way.
If you want to put an end to your back problems or get back into fitness in a sustainable way, I recommend you contact Andy!'
—Laurent Feraudet