







Almost every client that comes to me with low back pain has already failed to resolve it having seeing several other practitioners. Sometimes, their back pain has even been made worse by the clinicians they've seen. Despite this, I'm usually able to help them make significant improvements.
However, for transparency, I want to include cases of individuals I haven't been able to help, for varying reasons. These cases are relatively rarely, but they do occur.
Here are five examples:
1. Julie
Julie had been suffering with chronic low back pain on and off for over a decade. She had a disc bulge at L5-S1 and accompanying sciatic symptoms in her leg.
She also revealed to me that she'd had an eating disorder in her teens which had resulted in osteopenia (low bone density that weakens bones, making them more susceptible to fractures) in her hips and lower back.
She worked as a Pilates instructor, which had initially helped her pain, but since becoming a mother of two small children, it was no longer helping and had recently begun to actually make her pain worse.
Julie told me that she was in constant pain - she did not have any pain-free periods, only variations in intensity. However, she explained that her pain changed with different movements, postures and loads, so I decided it was appropriate to work with her.
We were able to find her a position of respite and established that her spine tolerated compression while it was in a neutral, stacked position. Yet, many movements were still painful, and she was also fearful about trying different exercises because previous exercise programs had always aggravated her pain.
Given the sensitivity of her spine, I recommended that she try a 'virtual surgery', as described by Stuart McGill in his book, Back Mechanic.
This is where the individual is led through the recovery program of a surgery patient without actually going under the knife. That way, they receive the forced rest that often benefits surgery patients more than the actual surgery (which is sometimes determined as the course of action based solely on MRI findings which may or may not be the actual generator of the individual's current pain).
In practice, virtual surgery means: no stretching, no gym, no picking up your kids, no cooking in the kitchen where you're forced to stoop over a counter, etc. All postures, movements and loads that stress the spine or provoke pain must be eliminated, and the only form of exercise allowed is usually walking.
In Julie's case, this would have forced her to give her spine the rest it needed to reduce its sensitivity before beginning to progressively strengthen it. There is strong evidence to suggest that individuals with osteopenia, and even osteoporosis can significantly improve their bone health with a combination of resistance and impact training, providing it's dosed appropriately.
However, as a single mum of two small children, and with no support from extended family, Julie was unable to engage in the 'virtual surgery' program. She was unable to give her spine the rest it needed for her to even begin rebuilding resiliency in her spine.
I have a no refund policy, but I made an exception for Julie. This was the only occasion I've ever had to refund a client for the remainder of a package because she was simply unable to follow my recommendations.
2. VJ

VJ flew over to Dubai to do an assessment with me. He had spent 18 months in prison in his home country, during which time he had been forced to sit and sleep on the concrete floor of a small cell. The constant pressure on his tailbone had left him with chronic low back pain and various associated symptoms.
Given that VJ wasn't a native English speaker, I conducted his assessment with the aid of a translator which made communication of nuances quite challenging. However, after careful questioning, while taking his personal history, we uncovered a total of three red flags for cauda equina syndrome. This is a medical emergency where the bundle of nerve roots at the base of the spine becomes compressed or damaged, disrupting motor and sensory signals to the legs, bladder, and bowel.
He explained that he was unable to urinate while standing, he had experienced low back pain with fever around one month before our assessment, as well as saddle anaesthesia a month before that. This was in addition to his patellar tendon and achilles reflexes being totally absent.
When I asked him if he had revealed these details to his doctors in his home country he told me he hadn't because he'd never been asked these questions before.
This was an urgent, medical issue, beyond my scope of practice. I recommended that VJ arrange a consult with a neurosurgeon as soon as possible.
3. Melody
Melody had a severe disc herniation at L5-S1 with significant loss of disc height. Her assessment revealed that she was shear-intolerant, flexion-intolerant, extension-intolerant and her joints were hypermobile.
Initially our main focus was to improve her spine hygiene and exercise technique that had no doubt contributed to her disc herniation. I made her aware of her hypermobility and designed a program to help stabilise her spine and hips.
We managed to get her to a point where she would have pain-free periods for a couple of weeks. Everything seemed to be going to plan. But, despite her improved spine hygiene and exercise technique, she continued to have flare-ups. She couldn't get rid of a deep, nagging pain that would increase in intensity at night.
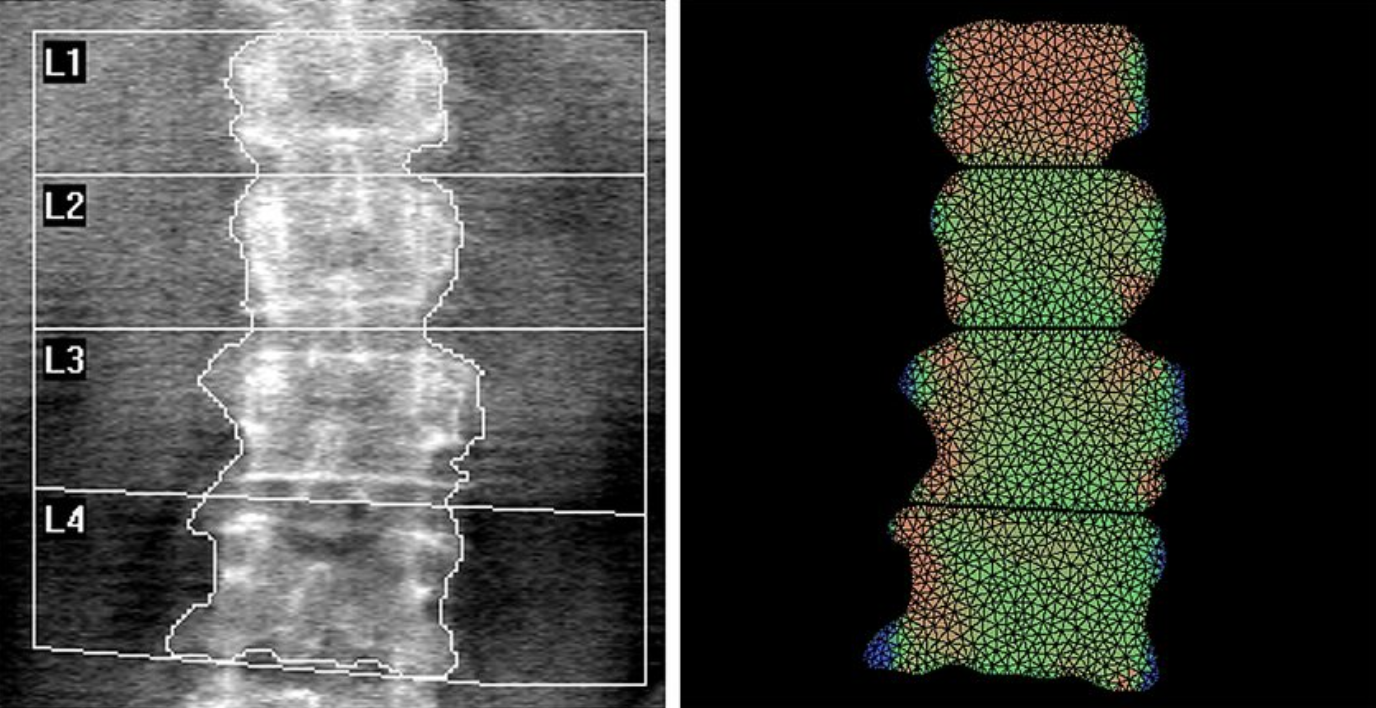
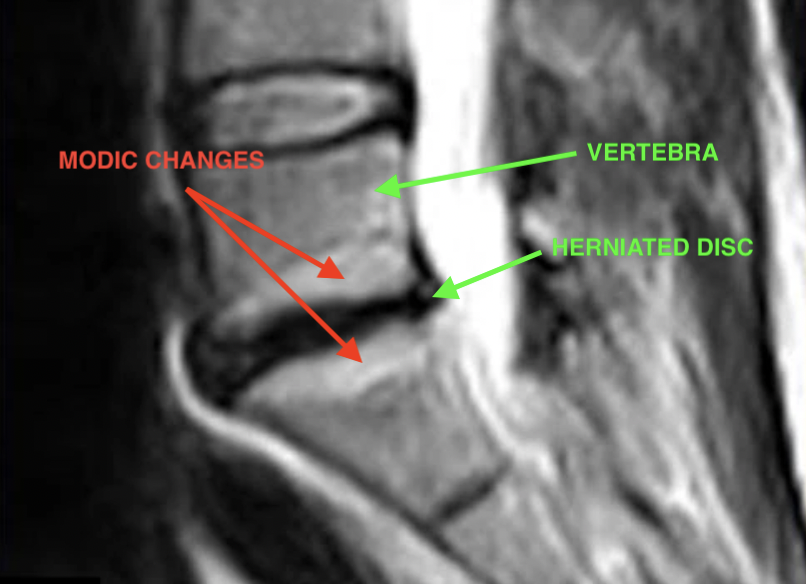
This did not fit the pattern of discogenic pain that she had previously. It suggested that another detail on her MRI, the Modic changes on the vertebrae either side of her disc herniation were her current source of pain.
Modic changes are bone oedema (bone bruising) resulting from fractures to the trabeculae of the vertebrae. The bone and bone marrow get corroded and are replaced by fibrovascular tissue (a liquid a bit like the puss in a blister).
She was considering surgery which had been recommended to her by two different surgeons. However, I was skeptical that this would resolve her pain.
After researching other options, Melody managed to organise a consultation with Dr. Hanne Albert, one of the world's leading researchers of Modic changes. Dr. Albert confirmed that Melody's Modic changes were the result of a bacterial infection that had entered her vertebrae via her herniated disc.
Surgery was not the solution. The solution was a trip to Denmark to start a 100-day course of antibiotics in conjunction with strict limitations on physical activity.
Melody recently completed her course of antibiotics and told me that her back is feeling the best it's been in a long time. She still has a long road ahead - the complete rehabilitation program usually takes around 2 years in total, but it has a 92% success rate.
*NOTE: this does not mean that if you have visible Modic changes on your MRI they are definitely the source of your low back pain. The plan of action should still be to identify your pain triggers and improve spine hygiene to reduce the stress on your spine. Sometimes this will be enough. However, sometimes, as in the case of Melody, it isn't.
Melody is an example of a fairly complex case where there were several factors contributing towards her pain. It only became clear that her Modic changes were the source of her pain once we had eliminated other factors.
4. John

John contacted me about his wife who had a severe scoliosis, and he wanted to know if I could help. After he explained to me about his wife's condition it seemed clear that although she had low back pain, her scoliosis appeared to be the root cause of this.
I recommended that his wife should see a Schroth practitioner before working with me. While I often have clients who have a mild scoliosis that's incidental to their low back pain, I am not a specialist in treating severe cases of scoliosis that are the primary cause of someone's pain. My policy is to refer out cases like these.
5. Dimitri

Dimitri is an amateur racing driver who competes in the 24h endurance race held in Dubai. He came to me with a disc bulge and low back pain that kept flaring up whenever he raced.
It was clear during his assessment that his spine couldn’t tolerate shear – the forces that provoke one vertebra to slide forwards and backwards on the one below.
This explained why he experienced pain when he braked hard in his car. With his legs and pelvis locked in place, braking forced his torso forward a short distance until the belts caught him.
Every hard stop was a little forward nudge of the vertebra at the level of his spine that couldn’t tolerate shear. Corner after corner. Lap after lap.
On top of that, he’s 6'2" in a tiny cockpit. Cramped hips, slightly flexed lower back, whole body vibrating and shunted around for hours. Not ideal conditions for a healing disc.
I explained to Dimitri that if he wanted his back to heal, he needed to eliminate ALL of his pain triggers, including racing his car. But stopping racing was out of the question for him.
So we tried to work around that. For six weeks we implemented a conservative program: building core endurance, tightening up spine hygiene, and getting rid of some of his gym exercises that were clearly making things worse.
He made fantastic progress and was doing well… until he got back in the car.
Unfortunately, the harsh reality is that sometimes your recovery plan doesn't align completely with what you want to do. And, it's not up to me to tell you what to sacrifice. You decide what you’re willing or not willing to give up. My job is to show you the cost, explain the trade-offs, and give you the best plan possible inside those boundaries.
But, you can't cheat physiology. If you don't provide your spine with the right conditions for it to heal, you shouldn't expect it to.
*All names have been changed to respect client anonymity.